Attorney-Approved Do Not Resuscitate Order Template for Virginia
In the realm of healthcare and personal decision-making, the Virginia Do Not Resuscitate Order form stands as a critical document for individuals seeking to make clear their desires concerning resuscitation in the event of a cardiac or respiratory arrest. This form, essential for those wishing to ensure their medical wishes are respected, serves as a directive to medical professionals and emergency responders, indicating that the individual does not want to be resuscitated through CPR (cardiopulmonary resuscitation) or advanced cardiac life support measures if their breathing stops or if their heart ceases to beat. The completion of this document requires thoughtful consideration and often, consultation with healthcare providers to fully understand the implications and ensure that the form accurately reflects the individual's wishes. The legal binding power of the Do Not Resuscitate Order ensures that patients' preferences are honored, offering peace of mind to them and their families during what is often a difficult and emotional time. By clearly stating one's choices regarding life-sustaining treatment, this form plays a pivotal role in the broader discussion about end-of-life care and personal autonomy in healthcare decisions.
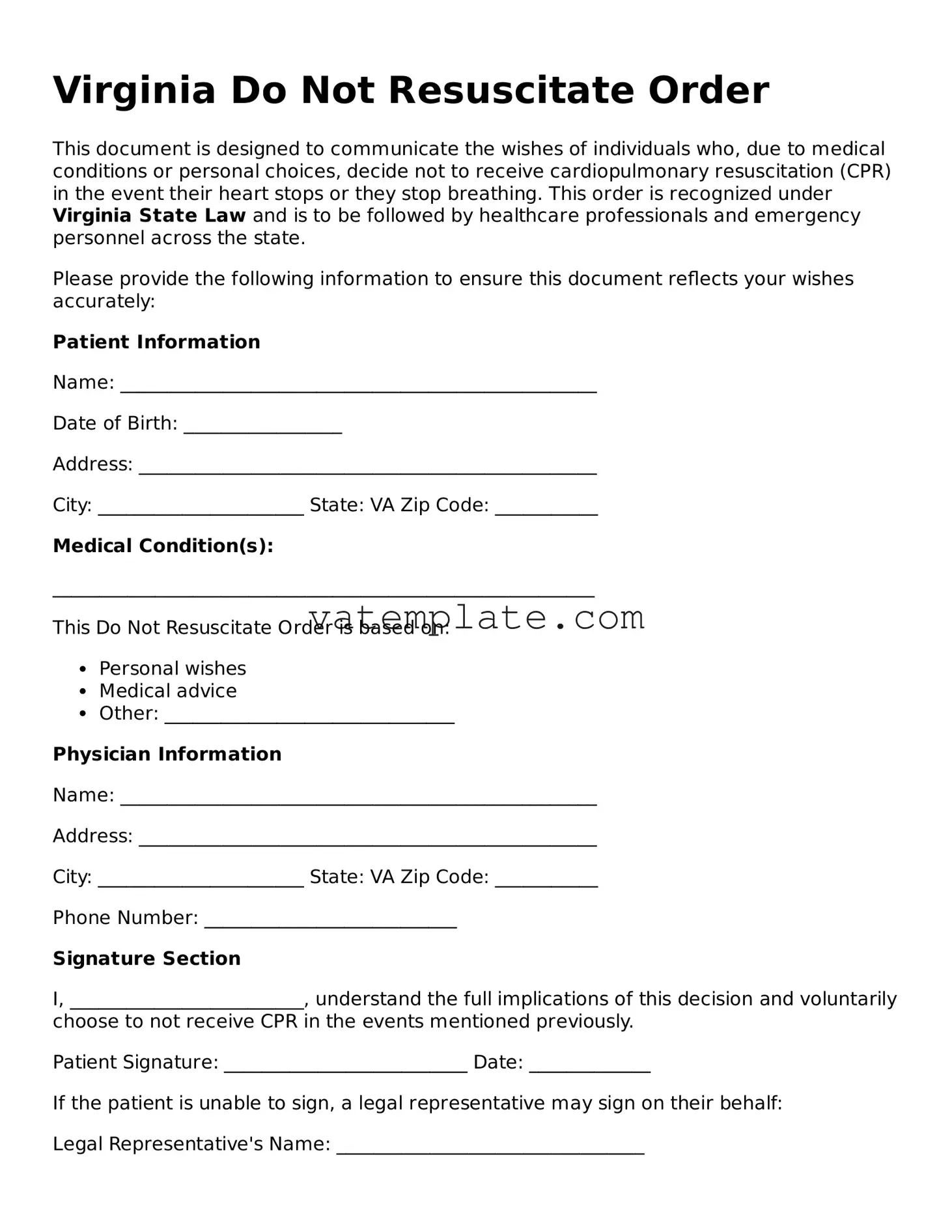
Virginia Do Not Resuscitate Order Example
Virginia Do Not Resuscitate Order
This document is designed to communicate the wishes of individuals who, due to medical conditions or personal choices, decide not to receive cardiopulmonary resuscitation (CPR) in the event their heart stops or they stop breathing. This order is recognized under Virginia State Law and is to be followed by healthcare professionals and emergency personnel across the state.
Please provide the following information to ensure this document reflects your wishes accurately:
This document should be kept in a place where it can be easily found by family members or emergency personnel. It is also recommended to discuss this decision with close family, friends, and healthcare providers to ensure that your wishes are known.
Note: This document can only be revoked by the patient or their legal representative and should be done so in writing.
Document Details
| Fact | Detail |
|---|---|
| Definition | A Virginia Do Not Resuscitate (DNR) Order is a medical directive that indicates a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event their heart stops or they stop breathing. |
| Governing Law | The DNR Order in Virginia is governed by the Virginia Health Care Decisions Act, which gives individuals the right to make decisions regarding their own health care, including the refusal of life-sustaining treatment. |
| Who Can Issue | A DNR order can be issued by a licensed physician. The physician must consult with the patient (if able) or the patient’s authorized health care agent or next of kin if the patient is incapable of making an informed decision. |
| Form Requirement | In Virginia, the DNR Order must be documented on a specific form approved by the Virginia Department of Health. This form serves as an official medical order. |
| Scope of Applicability | The DNR Order is applicable in various settings including hospitals, nursing homes, and in the patient's home. It is intended to communicate the patient’s wishes across different stages of care and various healthcare providers. |
Steps to Filling Out Virginia Do Not Resuscitate Order
Understanding the gravity of a Do Not Resuscitate (DNR) order is paramount for those in Virginia contemplating this crucial decision. This legal document instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) in the event that a patient's breathing or heartbeat stops. It is a deeply personal decision that should be made with careful consideration and, ideally, in consultation with healthcare professionals and loved ones. Once the decision is reached, filling out the Virginia Do Not Resuscitate Order form accurately is vital to ensure that your wishes are honored.
To complete the Virginia Do Not Resuscitate Order form, please follow these steps:
- Identify the Patient: Clearly write the full legal name of the person for whom the DNR order is intended. This ensures there is no confusion regarding the identity of the individual.
- Specify the Date of Birth: Enter the patient's date of birth. This is another crucial piece of information that helps healthcare providers confirm the patient's identity.
- Provide a Patient Number if Available: If the patient is currently admitted to a healthcare facility or has a unique patient or medical record number, include this information. It helps in matching the DNR order to the patient's medical records.
- Include the Date of Order: Fill in the date when the DNR order is issued. This date is essential for understanding when the order became effective.
- Physician's Information: The form must be signed by a licensed physician. Include the physician's name, license number, and contact information. This verifies that a medical professional has discussed the DNR order with the patient and/or the patient’s legal representative.
- Patient or Legal Representative Signature: The patient or their legal representative must sign the form, indicating their understanding and consent for the DNR order. If the patient is unable to sign, the legal representative’s signature is required, along with a statement of the patient’s condition that prevents them from signing.
- Witness Signatures: Two witnesses must sign the form, attesting that the patient or the legal representative willingly signed the DNR order. This helps to ensure the legitimacy of the process.
Once completed, it's crucial to keep the DNR order in a place where it is readily accessible to healthcare providers. Discussing your decision with family, close friends, and all relevant healthcare providers ensures that in the moment of need, your wishes are clearly understood and can be acted upon without delay. Remember, a DNR order is a significant and personal decision that impacts how end-of-life care is administered. It's recommended to review this decision periodically with healthcare providers to ensure that it continues to reflect your current healthcare wishes.
FAQ
What is a Do Not Resuscitate Order (DNR) in Virginia?
A Do Not Resuscitate Order (DNR) in Virginia is a legal document signed by a licensed physician that instructs health care providers not to perform cardiopulmonary resuscitation (CPR) if a patient's breathing stops or if the patient's heart stops beating. It is used by individuals who wish to forgo life-sustaining measures in the event of a cardiac or respiratory arrest. This document is part of a broader category of advance directives that allow individuals to outline their preferences for medical treatment in serious or life-threatening situations.
Who can request a DNR in Virginia?
In Virginia, a DNR order can be requested by:
- Any competent adult for themselves.
- A legally authorized representative for the patient, if the patient is a minor or not capable of making health care decisions.
- Parents or guardians of a minor child.
- Health care agents appointed through a valid Medical Power of Attorney, as long as it includes the authority to make end-of-life decisions.
How can one obtain a DNR in Virginia?
To obtain a DNR in Virginia, the following steps should typically be followed:
- Discuss your wishes with your physician. A DNR order must be medically justified, so it's essential to have a conversation with your healthcare provider about your health status and why you believe a DNR order is right for you.
- Your physician will need to sign the DNR order to make it official. In some cases, a nurse practitioner or physician assistant may also be authorized to sign a DNR, depending on state law and the specifics of your situation.
- Once signed, the DNR order should be kept in a location where it can be easily found by emergency personnel, such as on the refrigerator or in a wallet card form.
Is a DNR the same as a living will?
No, a DNR order is not the same as a living will. While both are types of advanced directives, they serve different purposes. A living will is a written document that details the types of medical care a person wishes to receive or avoid in the event they become unable to communicate their decisions due to illness or incapacity. In contrast, a DNR specifically addresses the issue of CPR and does not cover other forms of medical treatment.
Can a DNR order be revoked in Virginia?
Yes, a DNR order can be revoked at any time by the patient or their legally authorized representative in Virginia. This can be done in several ways, including:
- Orally expressing the wish to revoke the DNR order to a physician or another health care provider.
- Physically destroying the DNR order document.
- Writing a revocation statement and having it witnessed by someone other than a healthcare provider who is acting under the direction of the healthcare provider.
Does Virginia recognize DNR orders from other states?
Generally, Virginia health care providers honor DNR orders from other states, as long as they comply with Virginia's legal requirements for such orders. It is advisable for individuals with an out-of-state DNR to consult with a healthcare provider or a legal professional in Virginia to ensure their DNR is valid within the state. Being proactive can help prevent any confusion or legal issues that may arise in an emergency situation.
Common mistakes
Filling out a Virginia Do Not Resuscitate (DNR) Order form is a significant step for individuals making decisions about their end-of-life care. Yet, it's common for people to make mistakes during this sensitive process. Understanding these errors can help in completing the form accurately, ensuring that one's wishes are respected. Here are four common mistakes:
Not consulting with a healthcare provider: Before completing a DNR form, it's crucial to discuss it with a healthcare provider. This discussion ensures that the individual fully understands what a DNR order entails, including the medical implications of choosing not to have cardiopulmonary resuscitation (CPR) in the event of a cardiac or respiratory arrest. Skipping this step can lead to decisions that might not fully align with the individual's wishes or health status.
Incomplete information: A Virginia DNR form requires specific information to be considered valid. Sometimes people leave out essential details such as their full name, date of birth, or signature. Additionally, the form must be signed by a physician, nurse practitioner, or physician assistant. Missing information or signatures can render the document ineffective, leading to potentially unwanted medical interventions.
Not discussing the decision with family or loved ones: It is essential to talk about the decision to have a DNR order with family members or significant others. This conversation helps ensure that loved ones are aware of the individual's wishes, reducing confusion and distress in emergency situations. When families are unaware, they may inadvertently request medical interventions that go against the individual's DNR directive.
Failing to keep the DNR form accessible: After completing the DNR form, it's vital to keep it in an easily accessible location and inform family members, caregivers, and health care providers of its location. In an emergency, healthcare professionals need to locate the form quickly to comply with the individual's wishes. If the form is not readily accessible, medical staff may proceed with CPR and other life-sustaining measures by default.
In summary, properly filling out and managing a Virginia DNR form is a critical process that requires careful consideration and appropriate discussions with healthcare professionals, family, and loved ones. Avoiding these common mistakes can help ensure that an individual's health care preferences are clearly understood and respected.
Documents used along the form
In Virginia, the "Do Not Resuscitate Order" (DNR) is a critical document for patients who choose not to undergo CPR (cardiopulmonary resuscitation) in the event of a cardiac or respiratory arrest. Besides the DNR, healthcare providers, patients, and families may encounter several other forms and documents that complement or are closely related to a DNR. These documents play various roles from expressing healthcare wishes to outlining specific medical instructions for various conditions. Understanding these documents helps in ensuring a patient's healthcare preferences are well-documented and respected.
- Advance Directive: This document allows a person to provide instructions about their healthcare preferences, including end-of-life care, and to appoint a healthcare agent to make decisions on their behalf if they are unable to do so.
- Medical Power of Attorney: It designates a healthcare proxy, who is authorized to make medical decisions on behalf of the patient when they are incapacitated and unable to communicate their healthcare wishes.
- Living Will: Often part of an advance directive, it outlines which medical treatments a person wishes or does not wish to receive if they become seriously ill and cannot communicate their preferences about end-of-life care.
- POST (Physician Orders for Scope of Treatment) Form: Similar to a DNR but more comprehensive, this form outlines a patient's preferences for other life-sustaining treatments, such as feeding tubes or antibiotics, in addition to CPR.
- MOLST (Medical Orders for Life-Sustaining Treatment) Form: This is another form similar to POST used in some states, including preferences for CPR, ventilators, tube feeding, and other medical interventions.
- Healthcare Records Release Form: This form authorizes the disclosure of health information among healthcare providers, ensuring that a patient's healthcare team has access to necessary medical records, including their DNR order.
- Emergency Contact Form: Lists contacts to be notified in an emergency situation, including the healthcare proxy if one has been appointed, ensuring they can be reached quickly when needed.
- HIPAA Authorization Form: Authorizes the sharing of an individual’s health information with specified people, allowing family members or friends to receive updates about the patient’s medical condition.
- Organ and Tissue Donation Consent Form: Indicates a person’s wishes regarding organ donation upon death, which can be important for family members and healthcare providers to understand in the context of end-of-life care planning.
While the Virginia Do Not Resuscitate Order is a key document for those who wish to decline CPR, the other forms listed provide broader context and detail surrounding a patient's healthcare wishes. Collectively, they ensure a comprehensive understanding and respect for the patient's healthcare preferences, bridveauing gaps in communication among healthcare providers, patients, and family members. It's important for individuals to consider which documents best reflect their healthcare preferences and to discuss these preferences with loved ones and healthcare providers.
Similar forms
The Virginia Do Not Resuscitate Order form is similar to a number of other legal documents in terms of its purpose and implications for medical care. These documents, while distinct in their specific applications, share the common goal of respecting an individual's healthcare wishes, especially concerning life-sustaining treatments. Ensuring that patients' preferences are honored in critical situations is essential, and, like the Virginia Do Not Resuscitate Order, each document plays a crucial role in the process.
Living Will: Much like the Virginia Do Not Resuscitate (DNR) Order, a living will is a document that communicates an individual's wishes concerning end-of-life care. The primary similarity lies in their shared focus on ensuring that medical treatment aligns with the patient's preferences. However, while a DNR specifically addresses the refusal of CPR (cardiopulmonary resuscitation) in the event of a cardiac or respiratory arrest, a living will provides broader instructions regarding the types of life-sustaining treatments an individual does or does not want, such as mechanical ventilation, artificial nutrition, or hydration, if they become unable to communicate their wishes.
Medical Power of Attorney (POA): A Medical Power of Attorney is another document similar to the Virginia DNR in that it pertains to medical decisions and the patient's care preferences. The critical distinction between a Medical POA and a DNR is that the former appoints a healthcare agent or proxy to make health care decisions on behalf of the patient if they are incapacitated or unable to make decisions themselves. While a DNR is a directive with specific orders not to perform CPR, a Medical POA provides broader authority, allowing the designated agent to make a range of medical decisions, not limited to life-sustaining treatment, based on what they believe the patient would have wanted.
POLST (Physician Orders for Life-Sustaining Treatment): POLST forms closely resemble Virginia DNR orders in that they are both medical orders signed by a healthcare provider. Both documents are designed to ensure that the medical treatment provided aligns with the patient's wishes, especially in emergency situations or at the end of life. The key difference is that POLST forms are more comprehensive; they can include directives about CPR as well as other treatments such as antibiotics, intubation, mechanical ventilation, and feeding tubes. Therefore, while a DNR focuses strictly on CPR, a POLST covers a broader array of potential treatments and interventions.
Dos and Don'ts
When completing the Virginia Do Not Resuscitate (DNR) Order form, it is crucial to follow specific guidelines to ensure the document is valid and effectively communicates your wishes. Below are ten dos and don'ts to help guide you through this process:
Do:- Verify that the patient or their authorized representative is the one completing the form, to maintain its legality.
- Ensure that all information provided on the form is accurate and legible, to avoid any misunderstandings.
- Discuss the decision with a healthcare provider, to ensure that the choice is informed and reflects the patient's current health status.
- Include a witness's signature, as required by Virginia law, to validate the form's authenticity.
- Keep the original DNR Order in an easily accessible place, so that it can be quickly presented to healthcare personnel in an emergency.
- Inform family members, caregivers, and possibly close friends about the existence and location of the DNR Order, to prevent any conflicts during an emergency.
- Make copies of the completed DNR Order to distribute to your healthcare provider and any healthcare facilities where the patient receives care, ensuring all relevant parties are aware of the patient's wishes.
- Review and renew the DNR Order as necessary, especially if the patient's health condition changes, to ensure it reflects the patient's current wishes.
- Use a pen with blue or black ink for clarity and durability of the document.
- Consult with a legal professional if there are any questions or uncertainties regarding the DNR Order, to ensure it complies with Virginia laws.
- Leave any sections of the form blank, as incomplete forms may not be legally valid or respected by healthcare providers.
- Use pencil or any ink that can be easily erased or faded, as this can call the document's authenticity into question.
- Forge signatures or provide false information, as doing so is illegal and can invalidate the DNR Order.
- Fail to review the form for accuracy and completeness before finalizing, as mistakes can complicate or negate the DNR Order's effectiveness.
- Forget to date the form, as the date can be important for determining the order's relevance and recency.
- Ignore state requirements for witnesses or notarization, if applicable, as each state has its own laws regarding the execution of DNR Orders.
- Avoid discussing the decision with those close to you, as this can lead to misunderstandings or disputes in a crisis situation.
- Place the DNR Order in a safe or other secured location where it cannot be easily accessed in an emergency.
- Assume that a DNR Order is permanent and cannot be changed; patients or authorized representatives can revise it as needed.
- Overlook the requirement to communicate the existence of a DNR Order to all healthcare providers involved in the patient's care, as failure to do so could result in unwanted resuscitation efforts.
Misconceptions
When it comes to the Virginia Do Not Resuscitate (DNR) Order form, there are various misconceptions that individuals may have. Correcting these misunderstandings is crucial for making informed decisions about one's health care preferences. Below are seven common misconceptions about the Virginia DNR Order form:
It is only for the elderly: The DNR Order form is applicable to individuals of any age who wish to refuse resuscitation in the event of cardiac or respiratory arrest, not just to the elderly. This decision is based on personal values or medical advice, not age.
It applies in all medical situations: A DNR Order specifically addresses the refusal of cardiopulmonary resuscitation (CPR) in cases of cardiac or respiratory arrest. It does not apply to other medical treatments or emergency care unrelated to resuscitation.
It requires a lawyer to complete: While legal advice might be helpful in understanding the implications of a DNR Order, the form does not require a lawyer to fill it out. The patient, in consultation with their physician, can complete the form.
It is irreversible: A DNR Order can be revoked or cancelled at any time by the patient or their legal representative, ensuring that individuals have the flexibility to change their minds based on changing health conditions or personal wishes.
It guarantees no medical intervention will be given: A DNR Order only instructs healthcare providers not to perform CPR. Patients with a DNR Order will still receive all other appropriate medical care and interventions to relieve pain or address other health issues.
It takes effect immediately upon signing: For a DNR Order to be considered valid and effective in Virginia, it must be signed by the physician or other authorized healthcare provider in addition to the patient or their legal representative. This ensures a mutual understanding of the patient's wishes regarding CPR.
It is only for terminal illnesses: Individuals with or without terminal illnesses may choose to have a DNR Order based on their personal preferences, values, or specific medical advice. The decision is not limited to those with terminal conditions.
Understanding these misconceptions about the Virginia DNR Order form is essential for making empowered decisions regarding one’s healthcare preferences. It allows individuals to tailor their end-of-life care in a manner that aligns with their wishes and medical needs.
Key takeaways
Familiarity with the Virginia Do Not Resuscitate (DNR) Order form is essential for individuals wanting to make informed decisions about their emergency medical treatment preferences. Here are some key takeaways to guide you through filling out and using this form:
- Understanding the purpose: The DNR Order is used to instruct healthcare providers not to perform CPR (cardiopulmonary resuscitation) if a patient's breathing stops or if the patient's heart stops beating.
- Eligibility: Any individual can request a DNR Order, regardless of their health condition, though it is more common among patients with a terminal illness or those who are at a high risk of sudden cardiac arrest.
- Consultation is key: Before filling out the form, it’s crucial to consult with a healthcare provider. This discussion should cover the implications of a DNR Order and how it aligns with the individual's overall treatment plan.
- Legally binding: Once completed and signed, the Virginia DNR Order is legally binding. This means that medical personnel must respect the patient's wishes as stated in the document.
- Form requirements: Completing the form typically requires information about the patient, the medical condition leading to the request, and a signature from a licensed healthcare provider.
- The importance of witnesses: While not always mandatory, having the form signed in the presence of a witness or witnesses can lend additional validity and may be required in specific circumstances.
- Accessible documentation: It is paramount that the completed DNR Order is easily accessible to healthcare providers. Many people choose to keep it on their person or in a readily accessible place at home.
- Emergency services awareness: Informing local emergency services and caregivers of the existence of a DNR Order can ensure it is followed in an emergency.
- Duration and revocation: The DNR Order can be revoked at any time by the patient or their legally authorized representative. The process for revocation should be discussed with a healthcare provider.
- State-specific regulations: Virginia's DNR Order forms and regulations may differ from those in other states. It is important to use the correct form and follow state-specific guidelines.
Understanding these key points can empower individuals to make decisions that best reflect their healthcare preferences and ensure their wishes are respected in emergency situations.
Other Popular Virginia Templates
Example of a Quit Claim Deed Completed Virginia - Property developers often use Quitclaim Deeds for easy property consolidation or distribution without extensive warranties.
Virginia Divorce Laws - Pet custody arrangements can also be included, determining who will care for shared animals.
Self Proving Affidavit Virginia - For testators seeking peace of mind, attaching a self-proving affidavit to their will ensures their legacy is preserved as intended.